India’s healthcare sector has made significant strides but continues to face critical challenges such as infrastructure deficits, workforce shortages, and rising disease burdens. Various government policies and initiatives aim to address these issues to ensure accessible, affordable, and quality healthcare for all.
COVID-19 Exposed Weaknesses in the Healthcare Sector in India
COVID-19 exposed several weaknesses in India’s underfunded health system. Rural primary care is underfunded and has shortages of staff, equipment, drugs and infrastructure in many parts of the country. Urban primary healthcare has still not emerged as an active programme in many States. District and medical college hospitals suffer shortages of specialist doctors and support staff.

|
General facts about Health and Nutrition
|
|
Birth Rate (2021)
(World Bank)
|
- All India Level: 16 Live Births (per thousand of the population) ???? declining
|
|
Life Expectancy
(National Health Profile 2021)
|
- Average: 70 Years
- Females: 70 Years, Males: 67 Years
|
|
Infant Mortality Rate (IMR)
(NHFS – 5 (2019-21), SRS)
|
Current IMR: As per Sample Registration System (SRS) Bulletin of Registrar General of India (RGI) it is IMR is 30 per 1,000 live births in 2019 at National Level.
Target under National Health Policy – 28 by 2019.India reduced IMR by 42% over 11 years but still higher than global average (29)
- Differentials of rural (36) & urban (23) are still high.
|
|
Neonatal Mortality Rate (NMR)
(NHFS – 5, 2019-21)
|
- Current NMR: 25
- National Health Policy (NHP), 2017 goal for NMR: 16 deaths per 1000 live births by 2025. (With the current trend, India would fail to achieve this)
- SDG Goal for NMR: 12 deaths per 1000 live births by 2030
|
|
Maternal Mortality Ratio
(National Health Profile 2021)
|
MMR - As per Sample Registration System (SRS) data Maternal Mortality Ratio (MMR) is 97 per lakh live births in 2018-20.SDG target: 70 per 1,00,000 live births by 2030. Kerala (42), Maharashtra (55), and Tamil Nadu (63) have achieved this target. India on track to achieve the SDG target |
|
Total Fertility Rate (TFR)
(NFHS – 5, 2019-21)
|
- Overall TFR: 2.0 (Below Replacement Levels)
- States yet to achieve a replacement-level of fertility of 2.1: Bihar, Meghalaya, Uttar Pradesh, Jharkhand, and Manipur.
|
|
Sex Ratio at Birth (SRB) (NFHS – 5, 2019-21)
|
- Overall Sex Ratio – 1020 (increased from 933 in Census 2001)
- Sex Ratio at birth – 929
|
|
Proportion of institutional deliveries (NFHS - 5)
|
- Institutional Deliveries increased from 40% in 2005-06 to 88.6 % in 2019-21
- Target: 100% institutional Deliveries
|
|
Doctor Density
|
- India’s Doctor-population ratio: 1:834 (allopathic + AYUSH doctors)
- WHO’s recommended allopathic doctor-population ratio: 1:1000
Rural-Urban divide: Urban areas have 4 times as many doctors and 3 times as many nurses as compared to rural areas |
|
AYUSH
|
80% OF World’s Population rely on traditional medicine. (WHO) |
|
Disease Burden and Measures
|
|
Non-communicable diseases (NCD)
(WHO report)
|
- Global: NCD responsible for 70% of all deaths worldwide
- India: > 60% of all deaths in India can be attributed to NCDs.
- 1 in 4 Indians risks dying from an NCD before they reach the age of 70.
- Cancer, diabetes and heart diseases alone account for 55% of the premature mortality in India in the age group of 30?69 years.
- Main risk factors: Physical inactivity, tobacco use, excessive use of alcohol, unhealthy diets and Psycho-Social Stress.
- National Programme for Prevention & Control of Non-Communicable Diseases (NP-NCD)
- WHO’s Global action plan for the Prevention and Control of NCDs 2020 to 2030; Affordable Medicines and Reliable Implants for Treatment (AMRIT) Deendayal outlet, Jan Aushadhi stores, SDGs- reduce premature mortality from NCDs by one-third by 2030 (SDG 3.4)
|
|
HIV/AIDS
(SDG INDIA INDEX 2.0)
|
- People Living with HIV in India: 3rd largest HIV/AIDS population in world
- India’s HIV epidemic is slowing down: HIV incidence per 1000 uninfected population declined from 0.64 in 1995 to 0.07 in 2017.
- HIV and AIDS (Prevention & Control) Act, 2017; National AIDS Control Organization (NACO);
|
|
Tuberculosis (TB)
(Annual TB Report 2022)
|
- India is the highest TB burden country (28%) in the world and highest number of multi-drug resistant TB cases (WHO, 2019).
- HIV-associated TB: India has the second-highest number globally.
- TB-Mukt Panchayat Initiative;
- Ni-kshay Mitras have contributed over Rs 1,000 Cr, making it possibly the world’s largest community initiative for TB
- India is the only country in the world to implement a Sub-National Certification (SNC) exercise, a novel scientific method through which districts are verified for their progress of elimination
|
|
Food and Nutrition
|
|
Hunger & Malnutrition in India (NFHS- 5)
|
23% of women and 20% of men are undernourished
- >50% of pregnant women aged between 15 - 49 years are anaemic.
- >65% children under age of 5 years are anaemic.
Proportion of stunted children under 5 - 35% (global Average: 23%)
- Proportion of Underweight children - 30% (global Average: 13%)
- Proportion of wasted children - 20%
|
|
Obesity in India
(NFHS - 5)
|
- India is ranked as the third most obese nation in the world after the US and China
- 24% of women and 23% of men are overweight or obese
|
Issues and Challenges in the Healthcare Sector in India
India’s healthcare system has been battling various issues, including the low number of institutions and less-than-adequate human resources for quite a while now.
- Lack of Infrastructure: India has been struggling with deficient infrastructure in the form of lack of well-equipped medical institutes for quite a while now.
- For a considerable time, the government regulation mandated that private medical colleges must be built on at least five acres of land.
- As a result, quite a few private colleges were built in rural areas, where it became quite difficult to recruit adequately qualified, full-time doctors due to lack of proper living conditions, besides low pay scales.
- National Medical Commission (NMC) has put forward the idea to do away with the requirement of minimum five acres of land for setting up a medical college.
- Further, the commission has proposed to curtail the minimum number of beds required as a proportion of the number of seats in the college.
- Shortage of trained manpower: this includes doctors, nurses, paramedics and primary healthcare workers.
- The situation remains worrisome in rural areas, where almost 66 per cent of India’s population resides.
- The doctor-to-patient ratio remains abysmally low, which is merely 0.7 doctors per 1,000 people. This is compared to the World Health Organisation (WHO) average of 2.5 doctors per 1,000 people.
- Unmanageable load of Patients: Healthcare facilities had been feeling the strain due to unmanageable patient-load.
- In addition, there is the challenge to think beyond the obvious and promote virtual care protocols, and telehealth services, which can be leveraged to reduce the patient-load burden to a large extent.
- Public health policy and proactive healthcare: The latest National Health Policy (NHP) 2017 highlights the ‘Health for All’ approach to provide assured healthcare for all at an affordable cost.
- Ideally, the public health policy needs to be focussed towards proactive healthcare, not reactive healthcare.
- High out-of-pocket expenditure remains a stress factor: While public hospitals offer free health services, these facilities are understaffed, poorly equipped, and located mainly in urban areas.
- Most health services are, therefore, provided by private facilities, and 65 per cent of medical expenses in India are paid out of pocket by patients.
- Unregulated private sector: NITI Aayog has recently published the document, ‘Investment Opportunities in India’s Healthcare Sector’. This promotes further privatisation of health care in a country which already has one of the most privatised health systems in the world.
- The report fails to acknowledge the negative aspects of unregulated private health care; neither is there any mention of the need for regulation of private hospitals.

Government Initiatives for Strengthening the Healthcare Sector in India
- Anganwadi System: The Anganwadi system was established as part of the Integrated as Child Development Service (ICDS) programme, which has since been renamed Saksham Anganwadi and Poshan 2.0.
- Under the MoWCD, the Anganwadi Services Scheme is a centrally sponsored programme.
- It stands for one of the biggest and most distinctive early childhood care and development projects in the entire globe.
- Objectives: The program's objectives are to enhance the nutritional and physical health of young children (0–6 years), expectant mothers, and nursing mothers, as well as to lower the occurrences of mortality, morbidity, and malnutrition.
- System Depth: Through Anganwadi Centres (AWCs), Anganwadi Workers (AWWs), and Anganwadi Helpers (AWHs), the system provides services to 906.17 lakh beneficiaries.
- NATIONAL FAMILY HEALTH SURVEY-5 (NFHS) REPORT: NFHS-5 was released by the Ministry of Health and Family Welfare (MoHFW).
- Objective: To deliver accurate and comparable data on various topics, such as family welfare and health.
- The NFHS-5's scope is broadened by the inclusion of new dimensions like death registration, pre-school instruction, enlarged child immunisation areas, menstrual hygiene, etc.
|
Indicators
|
Findings
|
|
Total fertility rate, average number of children per woman
|
declined from 2.2 to 2.0
|
|
Institutional births
|
increased from 79% to 89% in India and in rural areas around 87% births being delivered in institutions and the same is 94% in urban areas.
|
|
Fully immunized
|
more than three-fourths (77%) children age 12-23 months, compared with 62% in NFHS-4.
|
|
Level of stunting
|
declined from 38% to 36%
|
|
prevalence of overweight or obesity
|
increased from 21% to 24% among women and 19% to 23% among men.
|
Right to Health in the Healthcare Sector in India
- Provisions in Constitution:
- Article 21: This article of the Constitution guarantees the right to life and personal liberty, which has been interpreted by the courts to include the Right to Health.
- DPSP: Part IV of the Constitution under the Directive Principles of State Policy (DPSP) (Articles 38, 39, 42, 43, & 47) ensures social and economic justice to its citizens directly or indirectly relating to public policy in terms of health putting the obligation on the state to ensure the effective realization of the Right to Health.
- Judicial Activism:
- Supreme Court in Paschim Banga Khet Mazdoor Samity case (1996) held that the primary duty of the government is to secure the welfare of the people being an obligation of the government to provide adequate medical facilities for its people in a welfare state.
- Supreme Court had ruled that every doctor whether at a government hospital or otherwise has the professional obligation to extend his services with due expertise for protecting life in Parmanand Katara Vs Union of India (1989).
- Human Dignity: The right to health is an essential component of human dignity and should be protected and promoted for all individuals, regardless of their gender, race, ethnicity, religion, or socioeconomic status.
- International Conventions: India is a signatory of the Article 25 of the Universal Declaration of Human Rights (1948) by the United Nations that grants the right to a standard of living adequate for the health and well-being to humans including food, clothing, housing and medical care and necessary social services.
Need of RTH in India
- Privilege to few: The right to equality guaranteed under Article 15 upholds non-discrimination on the basis religion, race, caste, gender, place of birth, etc. still the dismal investment in public health for decades has made healthcare a privilege available to a few.
- Break Discriminatory Structure: Right to health is critical to breaking discriminatory structures that will otherwise continue to perpetuate inequality in all spheres of life, including education, opportunity, wealth, and social mobility.
- Article 21’s Interpretation: The judicial interpretation of the right to life and liberty under Article 21 in several judgments as inclusive of health was crucial.
- As the universal access to healthcare is now as achievable as it is indispensable.
- Progressive Rights of the people: The rights of people are not stagnant, and must evolve as the country evolves.
- Service-Delivery Model: Ayushman Bharat is an ambitious scheme with great potential, but there is a difference between a right and a service-delivery model of development.
- Lack of Efficiency in healthcare: Healthcare facilities across the country lacks different levels of efficiency and sufficiency which can be outdone RTH.
- Dismal Primary Health Sector: RTH will help in developing the root of the healthcare sector i.e., the primary healthcare sector that lacks proper guidance and implementation of policies which makes people disbelieve in healthcare sector in India.
Arguments against RTH
- Due to the lack of clarity over who will be responsible for paying for the required free emergency treatment, private healthcare providers have been the most vocal opponents of the RTH.
- Critics claim that it is an attempt to surrender the State's duty to provide health protection and increases the burden of patients on the private sector.
- Many believe that the RTH will be unnecessary and highly restrictive.
- Without development or improvisation of the present structure of the healthcare facilities, implementing RTH will be devastating for already stressed medical field in India.
Challenges Related to Right to Health in India
- Inadequate Healthcare Infrastructure: India's healthcare infrastructure remains inadequate, particularly in rural areas where the 73% of the Indian population lack even basic medical facilities.
- Burden of schemes: Doctors are protesting against the RTH because they question the need for it when there are already schemes like Chiranjeevi that cover most of the population.
- Specialization concerns: They are also objecting to certain clauses, such as defining “emergency” and being compelled to treat patients outside their specialty as part of an emergency.
- High Disease Burden: India has a high burden of communicable and non-communicable diseases which requires significant investment in healthcare infrastructure and resources.
- Frontiers in Public Health Report: More than 33% of the individuals are still suffering from infectious diseases out of the total ailing population in India.
- Gender Inequalities: Women in India face significant health disparities.
- World Economic Forum 2021: India consistently ranks among the five worst countries in the world for the health and survival of females.
- Health Financing: Low levels of public spending on healthcare limits the government's ability to invest in healthcare infrastructure and resources, leading to inadequate healthcare services for individuals.
- Government of India spent 2.1% of GDP on healthcare in FY23 which is lower than the average health spending share of the GDP — at around 5.2% — of the Lower- and Middle-Income Countries (LMIC).
- No detailing of the process: To the charge that there is no detailing of the process, health rights activists have pointed out that it would be a function of the Rules, not the law itself.
- Concerns pertaining to compensation: Healthcare providers have a problem with reimbursement delays. Additionally, there are complaints that the predetermined package rates for various medical procedures and treatments are not sufficiently profitable or do not cover the actual cost.
Implementing Universal Health Coverage (UHC) in the Healthcare Sector in India
- Implementing Universal Health Coverage: As a critical indicator for human equity, security and dignity UHC makes sure that all people have access to the health services they need without the risk of financial hardship when paying for them.
- Health accessibility and affordability: A crucial healthcare problem even in the 21st century prompted World Health Organization to choose “Universal Health Coverage” as the theme for World Health Day 2019.
- India started working towards the universal problem of affordability and accessibility with the introduction of Ayushman Bharat.
Significance of UHC
- Universal health coverage has a direct impact on a population’s health and welfare.
- Access and use of health services enables people to be more productive and active contributors to their families and communities.
- Financial risk protection prevents people from being pushed into poverty when they have to pay for health services out of their own pockets.
- Universal health coverage is a critical component of sustainable development and poverty reduction, and a key element of any effort to reduce social inequities.
- Universal coverage is the hallmark of a government’s commitment to improve the wellbeing of all its citizens.
Issues and Challenges related to UHC
- Lack of Funds: Public sector is severely underfunded.
- Unaffordable Healthcare: Private sector is witnessing a high-cost healthcare service which is problematic.
- Regulation: Ineffective regulation is a concerned area.
- Poor Health Education: Lack of education and awareness regarding healthy lifestyles and preventive health measures can lead to an increase in preventable illnesses and conditions.
Government Steps for implementing UHC in Healthcare Sector in India
- National Health Policy (NHP) 2017: Allocating resources of up to two-thirds or more to primary care for achieving “the highest possible level of good health and well-being, through a preventive and promotive healthcare orientation”.
- A 167% increase in allocation for the Pradhan Mantri Jan Arogya Yojana (PMJAY) — the insurance programme which aims to cover 10 crore poor families for hospitalisation expenses of up to ?5 lakh per family per annum.
- The government’s steps to incentivise the private sector to open hospitals in Tier II and Tier III cities.
- Individual states are adopting technology to support health-insurance schemes. Example: Remedinet Technology (India’s first completely electronic cashless health insurance claims processing network) has been signed on as the technology partner for the Karnataka Government’s recently announced cashless health insurance schemes.
National Health Policy
National Health Policy: National Health Policy is an initiative by the Central Government to strengthen the health system in India covering various dimensions of health sectors like disease prevention, promotion of good health via cross-sectoral actions, health investment, strengthening human resources, technological advancements and more.
Launched in 2017 by the Central Government, has introduced four significant goals:
- Changing health priorities: Aims to tackle the increasing non- communicable and infectious diseases in India.
- Growth of the health care industry: Strengthen the health care industry by introducing technological advancement.
- Lower the expenditure: Aims to reduce medical expenses and provide superior services to poor and backward communities.
- Economic growth: Aims to enhance fiscal capacity by boosting economic growth.
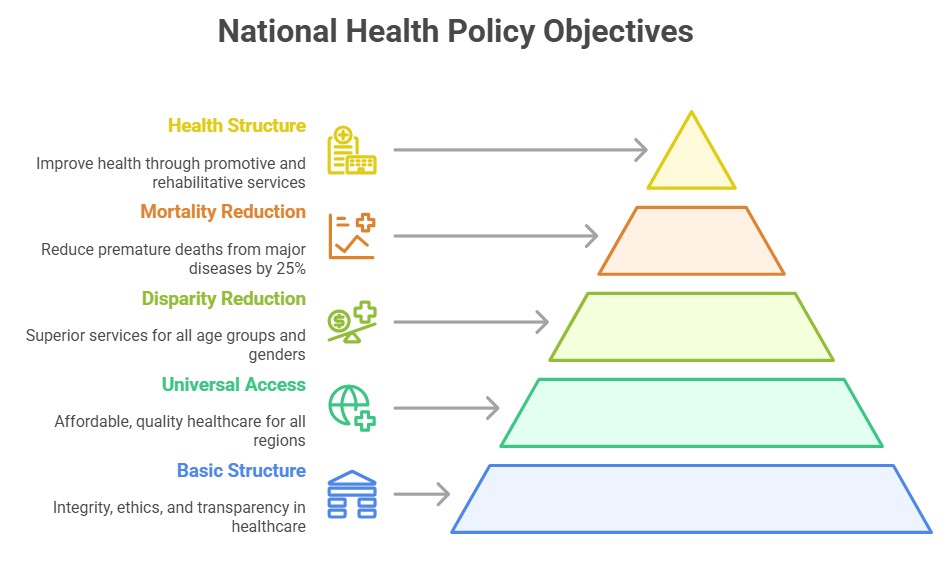
Objectives of National Health Policy
- Basic Structure: National Health Policy commits to integrity, highest professional standards and ethics integrating these functions in health care delivery services by maintaining transparency and a sustainable environment.
- Doing away Disparities: Aims to offer superior health services to every age group and gender.
- Universal Healthcare Services: Focuses on providing universal access to excellent quality health care services at an affordable price preventing regional disparities.
- Reducing Mortality Rate: Aims to reduce premature mortality from cancer, cardiovascular diseases, chronic respiratory diseases, and diabetes by 25% within 2025.
- Recognises the importance of sustainable development and time-bound quantitative goals.
- Developing Overall Health Structure: Aims to improve overall health structure through promotive, palliative, and rehabilitative services.
Drawbacks of the National Health Policy
- Repetition of Ideas: The new policy repeats several old ideas, and fails to fulfil 2015 promise of a Right to Health.
- It fails to make health a justiciable right in the way the Right to Education 2005 did for school education.
- Assurance-based Approach: The policies reference to an “assurance-based approach” abandons a radical change proposed in the draft policy of 2015 where National Health Rights Act aimed at making health a right.
- Disagreement with States: Health Ministry officials said the idea was dropped because state governments felt that health infrastructure was not yet at levels at which health could be made an entitlement, and the citizen could theoretically take a government to court for its denial.
- Diagnostics, drugs and essential health care services are already free in many states.
- Longevity in Implementation: The policy says that 2.5% GDP spend target for Health would be met by 2025 but the HLEG report of 2011, quoted by the 12th Plan document, had set the same target for the Plan that ends at the end of this march 2017.
- Health Cess: A health cess was a pathbreaking idea in the Health Ministry’s draft policy but now it has been rejected, with health officials maintaining that there is no dearth of funds.
Way Forward
- Increase Public Investment in Healthcare: The government should increase the budgetary spending on healthcare and allocate more resources to build a strong healthcare infrastructure.
- Enhancement of Health Expenditure: Health Expenditure which currently stands lower than most of the developing nations needs to be enhanced as a percentage of GDP.
- Prioritize Primary Sector: Strengthening the primary healthcare sector should be the priority.
- Expand Health Insurance Coverage: Expanding the health insurance coverage to all citizens would help reducing out-of-pocket expenses and make healthcare more affordable.
- Improve Healthcare Quality: The government should invest in improving the quality of care by developing quality standards, ensuring adherence to these standards, and providing training to healthcare providers.
- Invest in Health Information Systems: Priority should to given to develop robust health information systems that can provide timely and accurate data.
- Promote Preventive Healthcare: Focusing on preventive healthcare can reduce the burden of disease and the cost of healthcare.
Drug Regulation in India
India, has been mulling the creation of a mandatory recall law for substandard drugs since 1976, and yet no law exists that mandates such medicine be removed from the market to this day.
- In 1976, the Drugs Consultative Committee (DCC), which consists of all the state drug controllers along with senior bureaucrats from the Ministry of Health and the national drug regulator, the Central Drug Standard Control Organisation (CDSCO), discussed the issue of drug recalls.
- The issue of recalls came up again in meetings of the DCC in 1989, 1996, 1998, 2004, 2007, and 2011 but none of them resulted in amendments to the Drugs & Cosmetics Act to create a mandatory recall mechanism.
- Why has this issue been pending for so long in India with no redress?
- the Drug Regulation Section of the Union health ministry is simply not up to the task of tackling complex drug regulatory issues
- combination of different factors including apathy, lack of expertise in the area, and a greater interest in enabling the growth of the pharmaceutical industry than protecting public health.
- India’s highly fragmented regulatory structure, with each state having its own drug regulator.
- India’s drug regulators are aware of the fact that a mandatory drug recall system, which necessarily has to be centred on a system of wide publicity, will bring to public attention to the rotten state of affairs in India’s pharmaceutical industry.
- Dozens of drugs fail random-testing in government laboratories. Ideally, these drugs will be mandatorily recalled in a transparent manner, with the people being informed of the failures.
- Liberal punishments: Guidelines were first published by the Drugs Consultative Committee in 1993 and again in 2010. According to these recommendations, harassing medication makers would result from prosecuting every instance of inferior drugs. Therefore, the committee was established to carefully punish the producers.
- Necessity measures:

- The Union Health Ministry recently published a new draft Bill to replace the antiquated Drugs and Cosmetics Act, 1940.
- To create an effective recall mechanism, the responsibility of recalling drugs has to be centralised, with one authority that has the legal power to hold companies liable for failures to recall drugs from across the country.
- If India is a single market for drugs, it follows that it should have one regulator.
- The Drug and Cosmetics Act, 1940: imposes regulatory restrictions on the in-country production, distribution, and sale of medicines and cosmetics. The Act designates the sale of subpar medications as a serious violation since these medications have the potential to cause patients harm. A jail sentence or fine may be issued in accordance with this Act.
- Amend the Drugs and Cosmetics Act: The medications and Cosmetics Act's main objective is to prevent inferior medications from entering the market in the first place rather than to react to them after the fact. Therefore, the DCA must be changed to stop the production of inferior pharmaceuticals in the first place.
- Good Manufacturing Practices: Manufacturers ought to implement a rigorous system of quality control. Simple checks and balances must be followed, such as checking raw materials before incorporating them into drugs, purchasing raw materials from authorised producers, keeping equipment clean, etc. Any time there is a quality issue, a root cause analysis should be carried out right away.
Drug Regulation and Zero Tolerance Policy in the Healthcare Sector in India
The Centre has adopted a zero-tolerance policy towards narcotics
- According to the 2019 National Survey on Extent and Pattern of Substance Use in India, 2.26 crore people, or roughly 2.1% of the population, use opioids.
- Additionally, same poll revealed that 31 million Indians, or 2.8% of the population, used cannabis for bhang, ganja and charas.
Reasons
- Drug abuse has increased as a result of the breakdown of the united family system, a reduction in religious and moral values, and other factors, such as the desire to escape the harsh reality of life.
- Peer pressure: Many young people begin using drugs as a result of peer pressure from friends, teachers, or other members of their informal social networks.
- Easy Accessibility — India is positioned in such a way that the "Golden Triangle" and the "Golden Crescent" are to its east and west, respectively.
Initiatives:
- The MHA established the Narcos Coordination Centre (NCORD) system in 2016 to ensure efficient drug law enforcement.
- The portal serves as an efficient method for exchanging information amongst various institutions and authorities.
- The minister added that the Supreme Court is discussing the creation of fast-track courts and exclusive courts for the expeditious trial of drug cases.
Way Forward
India could reduce the treatment gap for mental disorders, increase the number of personnel in the mental health sector, work towards reducing discriminatory attitudes, and devise an integrated approach for detecting, treating, and managing patient needs.
- Corporate Social Responsibility (CSR) should be encouraged in the field of mental health.
Mental Health in the Healthcare Sector in India
Mental health issues are a major health challenge in the world today. According to the World Health Organization (WHO), there is a 10-25-year life expectancy reduction in patients with severe mental disorders. About 72% of member states had a standalone policy or plan for mental health in 2017.
- India introduced the National Mental Health Policy (NMHP) in 2014, and a rights-based Mental Healthcare Act in 2017, which replaced the Mental Healthcare Act of 1987.
- The NMHP, National Health Mission, National Adolescent Health Programme, and Ayushman Bharat have the necessary components to address the mental health issues of all sections of the population.
Issues and Challenges
- The share of mental hospitals per 1,00,000 population is as low as 0.01 in line with developing countries, according to the WHO.
- India was at the 99th position in the distribution of mental health outpatient facilities (per 1,00,000 population), with 0.18 units per 1,00,000 population.
- India was also at the 64th position in the distribution of mental health day treatment facilities
- The distribution of community residential facilities globally for the median year 2016 showed India at the 58th position, with 0.017 units per 1,00,000 population among the WHO member countries.
- Mental Illness: Mental illnesses include anxiety disorders, psychotic disorders, mood disorders, substance use disorders, personality disorders and eating disorders.
- The suicide rate was 10.6 per 1,00,000 population whereas in India, it was 16.3 per 1,00,000 in 2016.
- The suicide rate was higher among males compared to females.
- Mental health facilities: There are also challenges regarding funding, delivery of mental health packages, lack of trained staff, etc.
Government Initiatives

- Mental Healthcare Act, 2017
- The Act ensures healthcare for people suffering from mental illness through health services funded by the Government. It decriminalises suicide, disallows sterilisation.
- As part of Section 19, the government was made responsible for creating opportunities to access less restrictive options for community living — such as halfway homes, sheltered accommodations, rehab homes, and supported accommodation.
- Under the MHCA, all States are required to establish a State Mental Health Authority and Mental Health Review Boards (MHRBs) – bodies.
- While Ayushman Bharat allows for insurance for medical treatment of the mentally unwell, financial protection in the form of allowances should be initiated.
- National suicide Prevention Strategy: The Ministry of Health and Family Welfare’s recently published National Suicide Prevention Strategy fits right there.
- The most common reasons include family problems and illnesses, while other causes include marital conflicts, love affairs, bankruptcy, substance abuse and dependence.
- In India, more than one lakh lives are lost every year to suicide. In the past three years, the suicide rate has increased from 10.2 to 11.3 per 1,00,000 population.
- The Strategy also intends to write in mental health in the curriculum in educational institutions within the next eight years.
- It also lists interventions that have reduced the suicide rate in various sections in the country, including among students and rural groups, by limiting the availability of pesticides.
Conclusion
There needs to be a road map for mental health awareness. This should include the traditional media, government programmes, the education system, industry, and social media. Media awareness and government involvement is already happening in India but both can improve. It is high time that industry and private sector companies set up counselling facilities.